Skills Assessment is Not Competency
Why Understanding What Competency-Based Education Truly Is, Matters
Discovering the pivotal distinction between skill assessment and competency can help organizations better understand how to more effectively achieve their educational and training objectives.
Understanding the difference not only reveals a more strategic approach to student progress and professional development but also underpins the foundation of successful healthcare education and outcomes.
Understanding the Difference Between Skills Assessment and Competency
Skills Assessment
Skills assessment traditionally encapsulates an evaluation of an employee’s or student’s capability to execute a certain task, often narrowed down to particular job or curriculum requirements.
Mastery of Specific Skills

Skills assessment has been traditionally viewed as a method for gauging an employee’s or student’s proficiency in performing specific, delineated tasks. The process involves evaluating and measuring an individual’s technical skills—frequently using tests, performance evaluations, or practical examinations—to determine their capacity to carry out the duties or objectives that are considered crucial for a specific position or course of study.
Traditionally, skills assessments aim to ascertain that the individual has mastered the mechanics necessary for a given task. For instance, in a clinical healthcare setting, a skills assessment might test a nursing student’s competence in administrating injections.
Focus on Skill Sets
Skills assessment can be pinpointed and singular, focusing on a particular skill set without necessarily considering the broader implications or associated soft skills. For example, in evaluating a student’s skill in mathematics, the assessment would typically measure their ability to solve equations but may not assess their ability to apply mathematical reasoning in real-world scenarios.
Contrasting with a more integral approach to personnel evaluation, a comprehensive skills assessment can often miss the broader aspects of an individual’s capabilities such as critical thinking, adaptability, and problem-solving, which are increasingly valued in modern educational and professional settings.
Competency Assessment
Competency assessment, in contrast, captures a broad-spectrum proficiency that aligns with comprehensive knowledge bases and identifies critical skill gaps.
The Holistic Approach
Competency assessment, as a counterpoint to traditional skills assessment, embraces a wide-ranging evaluation of proficiency that is deeply integrated with a broad spectrum of knowledge across various domains, ensuring alignment with extensive educational or professional objectives. Unlike the narrower approach of skills assessment, competency assessment in healthcare training is designed to ascertain not only whether individuals can perform specific clinical procedures but also whether they understand underlying theories, can apply knowledge to unique situations, can make informed decisions under pressure, and are adept in the coordination of care across interdisciplinary teams.
This holistic appraisal looks to address the critical skill gaps that can significantly impact patient outcomes and the efficiency of healthcare services. It is pivotal in contexts such as nursing education, where it’s not sufficient to merely perform tasks – practitioners must exhibit comprehensive judgment and adaptability in high-stakes environments. Competency assessments often include evaluations of soft skills such as communication, empathy, and leadership, alongside the hard skills associated with clinical care.
Looking at Every Aspect of the Learning Process
 Effective competency assessment necessitates a multi-modal approach, leveraging various tools such as simulation labs, objective structured clinical examinations (OSCEs), and portfolio reviews. These modalities enable educators and evaluators to capture a three-dimensional perspective of a healthcare professional’s abilities, including cognitive (knowledge), psychomotor (skill), and affective (attitude) domains.
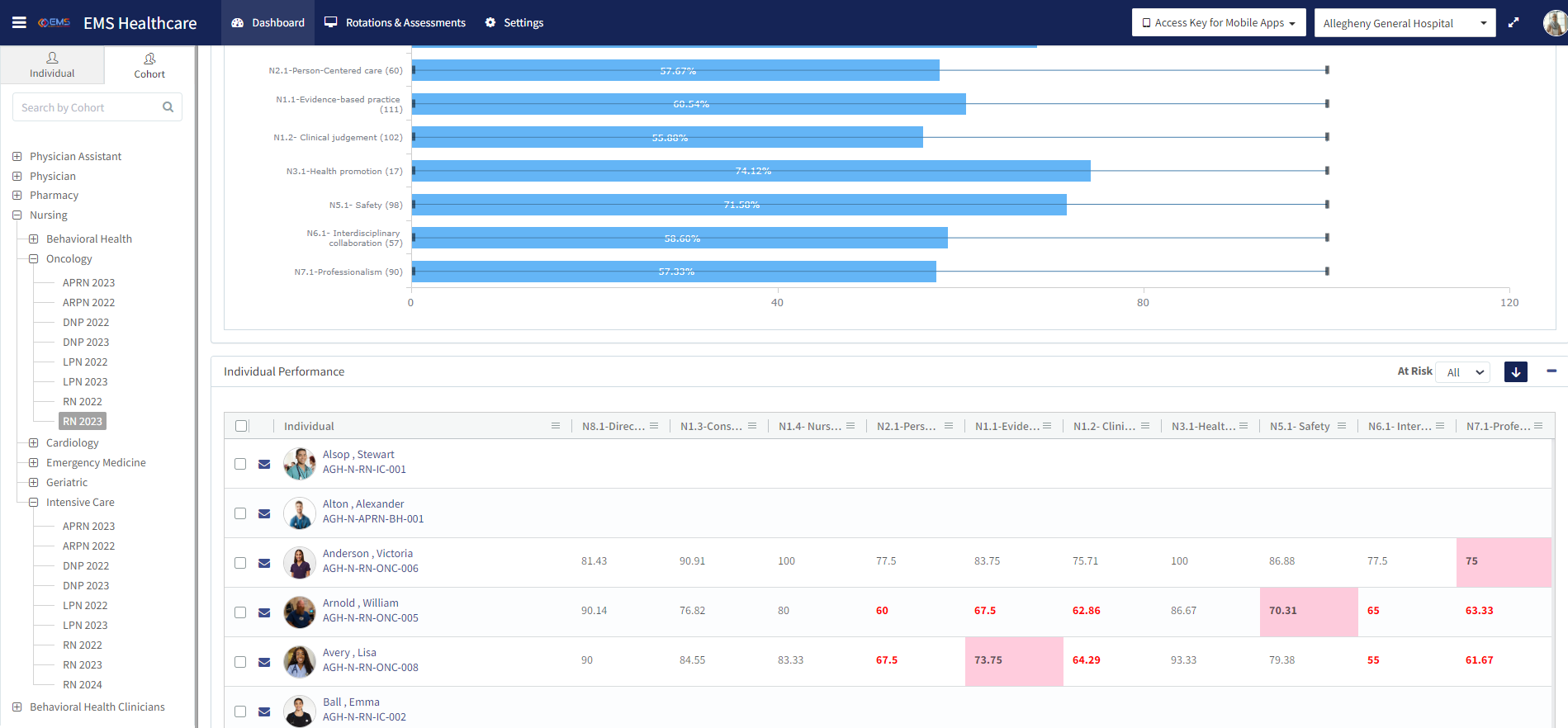
In the realm of healthcare training, competency assessment has gained traction not only because of its comprehensive nature but also due to its predictive value in professional practice. Health systems that prioritize competency assessment can more readily identify and intervene in areas where practitioners may need additional training, thereby elevating the standard of care delivered and contributing to improved patient safety and quality improvement.
Furthermore, the alignment of competency assessment with healthcare accreditation standards, regulatory requirements, and evidence-based practice underscores its importance. These assessments can provide data to inform curriculum development, continuing education, workforce planning, and policy-making, reflecting a dynamic and responsive approach to the complex landscape of healthcare training and practice.
Effective competency assessment necessitates a multi-modal approach, leveraging various tools such as simulation labs, objective structured clinical examinations (OSCEs), and portfolio reviews. These modalities enable educators and evaluators to capture a three-dimensional perspective of a healthcare professional’s abilities, including cognitive (knowledge), psychomotor (skill), and affective (attitude) domains.
In the realm of healthcare training, competency assessment has gained traction not only because of its comprehensive nature but also due to its predictive value in professional practice. Health systems that prioritize competency assessment can more readily identify and intervene in areas where practitioners may need additional training, thereby elevating the standard of care delivered and contributing to improved patient safety and quality improvement.
Furthermore, the alignment of competency assessment with healthcare accreditation standards, regulatory requirements, and evidence-based practice underscores its importance. These assessments can provide data to inform curriculum development, continuing education, workforce planning, and policy-making, reflecting a dynamic and responsive approach to the complex landscape of healthcare training and practice. 
The Core Pillars of Competency
There is an emphatic delineation of ‘competency’ from mere ‘skill assessment’. Competencies encompass a multifaceted matrix:
Knowledge
Skill
Ability
Behavior
Empower Healthcare Education with Comprehensive Knowledge
 In healthcare education, knowledge encompasses understanding a wide array of subjects, including human anatomy, pharmacology, pathophysiology, and healthcare policies, among others. This information is acquired through rigorous study and investigation, often involving a blend of classroom learning and hands-on experiences such as clinical rotations. For instance, a nurse must not only learn about different diseases and their treatments but also understand the underlying physiological mechanisms to provide appropriate patient care and education. The depth and breadth of knowledge acquired lay the groundwork for all subsequent clinical competencies.
In healthcare education, knowledge encompasses understanding a wide array of subjects, including human anatomy, pharmacology, pathophysiology, and healthcare policies, among others. This information is acquired through rigorous study and investigation, often involving a blend of classroom learning and hands-on experiences such as clinical rotations. For instance, a nurse must not only learn about different diseases and their treatments but also understand the underlying physiological mechanisms to provide appropriate patient care and education. The depth and breadth of knowledge acquired lay the groundwork for all subsequent clinical competencies.
Enhance Skill Development in Healthcare
 Skill development in healthcare revolves around the ability to apply theoretical knowledge to perform specific tasks proficiently and safely. This includes both technical skills—such as administering injections, suturing wounds, or conducting physical examinations—and softer skills, like effective communication with patients and families. Skill proficiency in healthcare is achieved through repetitive practice, typically in a supervised setting where feedback from experienced professionals can guide improvements. Simulations and clinical practicums are integral components of healthcare education, providing a controlled environment for students to refine their skills.
Skill development in healthcare revolves around the ability to apply theoretical knowledge to perform specific tasks proficiently and safely. This includes both technical skills—such as administering injections, suturing wounds, or conducting physical examinations—and softer skills, like effective communication with patients and families. Skill proficiency in healthcare is achieved through repetitive practice, typically in a supervised setting where feedback from experienced professionals can guide improvements. Simulations and clinical practicums are integral components of healthcare education, providing a controlled environment for students to refine their skills. Augment Learner Abilities
 In the healthcare sector, ‘ability’ pertains to both the innate and developed capacities that enable individuals to carry out their roles effectively. This includes cognitive abilities, such as critical thinking and problem-solving, which are crucial for diagnosing conditions and planning patient care; emotional intelligence, which aids in empathetic interactions with patients and families; and physical abilities, necessary for performing procedures or managing the demands of long shifts. Healthcare education programs often incorporate scenario-based learning and case studies to cultivate these abilities, enabling students to analyze complex situations and make informed decisions.
In the healthcare sector, ‘ability’ pertains to both the innate and developed capacities that enable individuals to carry out their roles effectively. This includes cognitive abilities, such as critical thinking and problem-solving, which are crucial for diagnosing conditions and planning patient care; emotional intelligence, which aids in empathetic interactions with patients and families; and physical abilities, necessary for performing procedures or managing the demands of long shifts. Healthcare education programs often incorporate scenario-based learning and case studies to cultivate these abilities, enabling students to analyze complex situations and make informed decisions. Cultivate Appropriate Behavioral Competencies
 Behavior in healthcare education refers to the observable responses of individuals in clinical settings, reflective of their professionalism, ethical standards, and personal attitudes. This encompasses how healthcare providers interact with patients, colleagues, and other stakeholders; adhere to privacy laws and ethical guidelines; and manage stress or conflict. Cultivating appropriate behavioral competencies involves instilling a strong sense of responsibility, patient-centered care, and teamwork from the early stages of training. Educational programs often include behavioral assessments and reflections as part of the curriculum to help students internalize the values and norms of the healthcare profession.
Behavior in healthcare education refers to the observable responses of individuals in clinical settings, reflective of their professionalism, ethical standards, and personal attitudes. This encompasses how healthcare providers interact with patients, colleagues, and other stakeholders; adhere to privacy laws and ethical guidelines; and manage stress or conflict. Cultivating appropriate behavioral competencies involves instilling a strong sense of responsibility, patient-centered care, and teamwork from the early stages of training. Educational programs often include behavioral assessments and reflections as part of the curriculum to help students internalize the values and norms of the healthcare profession. Healthcare education’s focus on this multifaceted matrix of competencies ensures that graduates are not just technically proficient but also capable of delivering compassionate, ethical, and high-quality care. The integration of knowledge, skill, ability, and behavior forms the cornerstone of professional practice that upholds patient safety and improves health outcomes.
Why Competency is King
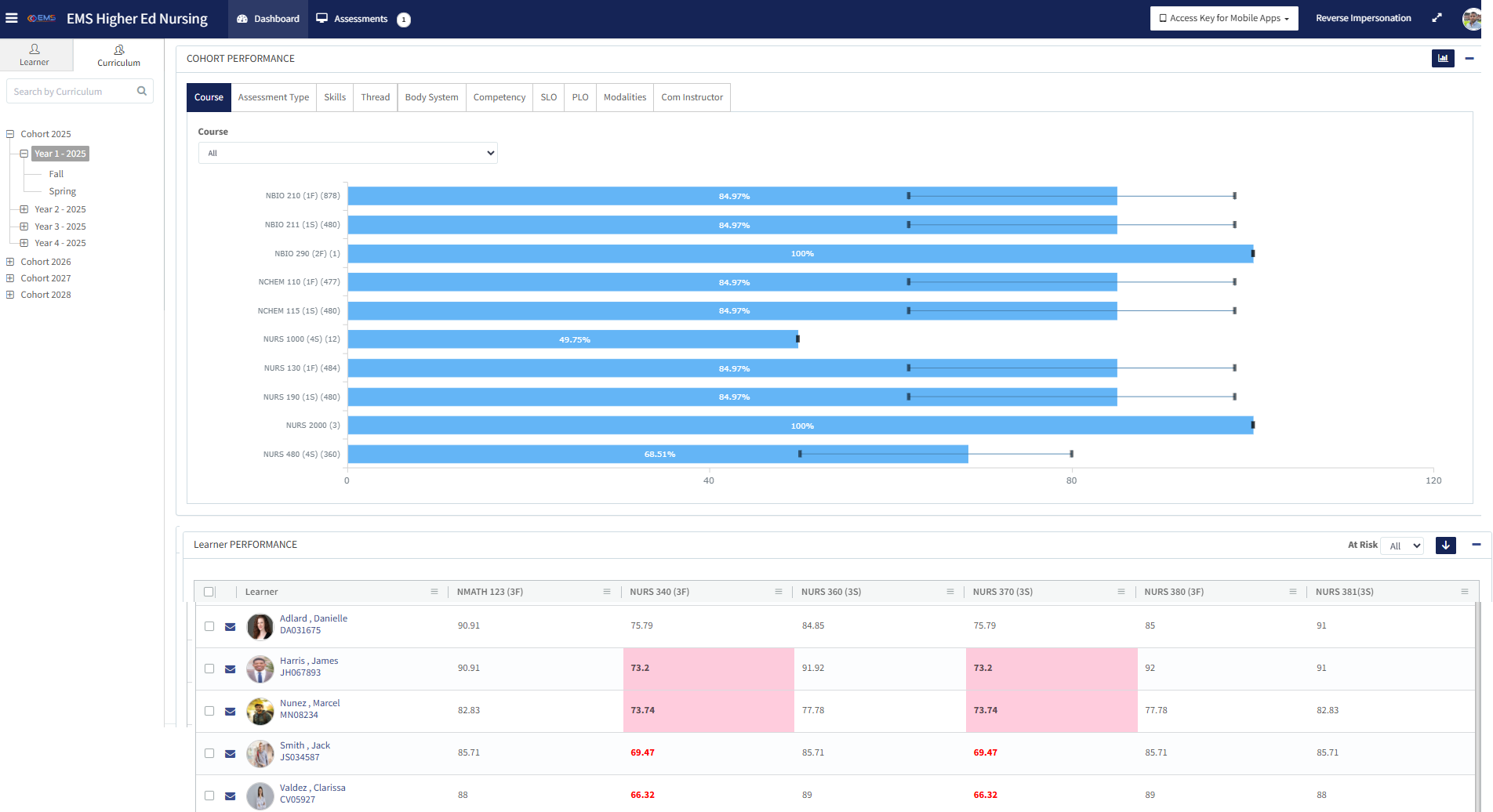
In health systems, proficiency targets associated with competency levels are designed to flexibly meet both an individual’s role and the organization’s strategic imperatives while for healthcare education, student progression can be meticulously aligned with competency levels to appreciably improve learning outcomes. This underscores the intrinsic value of viewing competency as a broad, developmental construct that goes beyond mere skills assessment to include a holistic approach to professional growth and organizational alignment. Here’s why:

Flexibility to Meet Individual and Organizational Needs
Competencies in health systems are not static; they are dynamic and tailored to accommodate the varying roles within the healthcare workforce and the strategic goals of the organization. This adaptive approach ensures that healthcare professionals are not just assessed on isolated skills but are also evaluated on their ability to integrate and apply a comprehensive set of competencies that support both their professional growth and the healthcare organization’s mission.
For instance, a competency framework might include leadership and teamwork, which are essential for navigating the complexities of healthcare delivery, contributing to the organization’s adaptability, efficiency, and patient care quality.
Meticulous Alignment with Educational Progress
In healthcare education, the emphasis on competencies allows for a more structured and intentional design of educational programs. By clearly defining competency levels, educators can align curricula, teaching methods, and assessment strategies to sequentially build students’ capabilities across knowledge, skill, ability, and behavior.
This alignment ensures that learning outcomes are not just about mastering specific tasks but about cultivating a well-rounded professional who can think critically, act ethically, and adapt to various clinical situations. Through competency-based education, students can chart their progress in a more meaningful way, understanding not only what they need to learn but also why, and how it applies to their future roles as healthcare professionals.
Improvement of Learning Outcomes
The ultimate goal of integrating competency frameworks into healthcare education and professional development is to improve learning outcomes and, by extension, enhance patient care quality. By focusing on the development of comprehensive competencies that encompass knowledge, skills, abilities, and behaviors, healthcare professionals are better equipped to meet the challenges of modern healthcare delivery. This holistic approach to competency development acknowledges that high-quality patient care requires more than technical proficiency; it demands a blend of scientific knowledge, technical expertise, critical thinking, ethical reasoning, and interpersonal skills.
Moving to Competency and Beyond
When presented with all of the information, it becomes evident that competency transcends mere skills assessment. Competency is about fostering a well-rounded, adaptable, and proficient healthcare workforce that can meet individual patient needs, adapt to the evolving healthcare landscape, and contribute to the overarching goals of healthcare organizations. It’s about charting educational and professional trajectories that respond to the complexities of healthcare, prioritize lifelong learning, and uphold the highest standards of patient care.
Schedule a Discussion
Take charge of your programs and maximize efficiency
with seamless end-to-end simulation management.
Click the Button to Get Started